

Oliver's Story
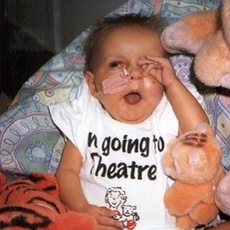
4th September. Oliver's Due Date. Today should have been Oliver’s due date. Instead he’s celebrating being 100 days old, in hospital.
Oliver was born at 25+6 weeks after I spontaneously went into labour. He was born at Birmingham Women’s Hospital, an hours drive from Leamington Spa where we live and weighed 2lb 1 oz.
Oliver spent his first 5 weeks in Birmingham where he spent time on and off the ventilator until he was stable enough and until a cot became available at Coventry University Hospital. In Coventry Oliver thrived and was steadily gaining weight and increasing milk feeds as well as slowly coping with less support breathing and moving from CPAP to high flow and then low flow.
We started to regain some normality in our upside down world and things looked good.
When Oliver was 7 weeks we got a phone call, asking us to come in straight away as Oliver was unwell. Oliver had been put onto an oscillating ventilator to help him breathe as his tummy had become so distended his lungs had collapsed. The doctors suspected he had an obstruction or possibly Necrotising Enterocolitis (NEC). We were told he urgently needed surgery but we may have to travel up to 2 hours away as Birmingham Children’s Hospital and Leicester Royal Infirmary did not have space. Thankfully Leicester Royal Infirmary were able to make a space. The transport team arrived who were reluctant to transfer Oliver and were told it was highly unlikely Oliver would make the journey as he was so poorly and his chances at surviving a major operation was slim.
We said goodbye to Oliver and made our way to Leicester not knowing if he would survive the journey.
Oliver made the journey and survived surgery where half of his small bowel was removed due to NEC. NEC is very common in premature babies and causes their gut to become diseased and die. It causes high levels of infant morbidity and the causes are still largely unknown. He was still very critical and needed a lot of support and several more blood transfusions and at last count had had 9 transfusions. He had a stoma created and after 2 weeks the stoma was looking less healthy and the decision was made to take him to theatre to insert a broviac line and also look at his tummy again. A further 10-15cm of dead bowel was removed and within days Oliver’s stoma began working and his condition improved.
Now 100 days old Oliver can only tolerate minimal feeds due to his short bowel and his main source of nutrition comes from TPN which is given intravenously. 2 weeks ago Oliver had laser treatment for ROP, eye disease common in premature babies.
We’d hoped to have Oliver home for his due date, Paul’s birthday in October and then Christmas. We were told yesterday this is not possible so we will have several more months of this. He is now outgrowing the neonatal unit and will soon be moved to a paedeatric ward until his stoma is reversed in 2-3 months. Once his stoma is reversed we will hopefully have a better idea of how well he will be able to absorb food and how long he will need TPN for…and when we can finally get our boy home.
Read more about Oliver and follow his progress here.


Aaron's Story
You never think for a moment that your unborn child you've carried around as part of you for all those months whilst pregnant could be anything other than perfect.
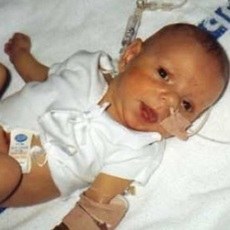
Born in Scotland, induced 3 weeks pre-term, due to "baby not growing" and delivered via an emergency C-section in August 1996, it was discovered our new born baby boy had a heart murmur, which was not too worrying for us as my nephew has a hole in his heart. He was transferred to our local children’s hospital in Edinburgh where they found out just how bad things were, he had a congenital heart disorder called Tetralogy of Fallots (4 defects) and required immediate surgery.
I was transferred to a maternity hospital elsewhere in the city; it was such a traumatic experience to be separated from my newborn baby. So at a ripe wee age of 6 days old our baby boy, now named Aaron, underwent his 1st of many surgeries. As a direct consequence of his surgery combined with his low birth weight Aaron developed something called NEC (Necrosising Enteral Colitus) which destroyed 3/4 of his small intestine leaving him with practically no absorption. He was put on artificial feeding via a gastrostomy and an IV line into his chest giving him TPN (Total Parental Nutrition)
Aaron remained in hospital, it took its toll on us, travelling up and down from the hospital, but we thought, ”Hey this TPN is the best thing since sliced bread.”
But it wasn’t for Aaron, at 8 months old his liver was so damaged with a liver disease called cholestasis due to this wondrous TPN being toxic to his liver and the fact that very little food was being absorbed via his gut…his feed either erupted up or blasted out.
We were informed by his consultant that we were facing not only the prospect of a small bowel transplant but now a liver transplant too.
Aaron’s 1st transplant assessment was down in Birmingham Children’s Hospital in the Spring of 1997 where it was agreed by all that Aaron most definitely required both organs and was put on the transplant list. They had only ever done a handful of these transplants in the UK...very scary, very daunting...only for us to be informed 1 week later that he couldn’t remain on the list as he wouldn’t have withstood the transplant surgery his heart was too weak and required further corrective heart surgery…we were devastated.
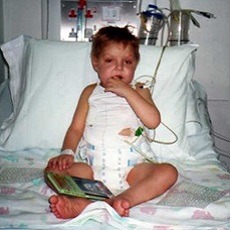
To be ”fit and well” enough for this necessary surgery was something Aaron was never going to be…or so we thought. We fought to get our little son home with all his pumps and medical equipment and when we finally got to take our baby boy home for the 1st time in his little life he was 13 months old in September 1997, he weighed that of a new born, just 11lb. We needed to be trained medically for about 3 weeks to cope with all Aaron’s needs!
He was to all involved... sent home to die!
I was crazy enough to have fallen pregnant during this living nightmare of ours, and Aaron’s baby brother Jamie was born in January 1998 but he became a wonderful breath of life and a positive distraction in our home he became a source of love and fun for Aaron. We tried to encourage Aaron to eat but because he never had nor for that matter ever had the need or urge to eat food we were so excited when he’d have a teaspoon of tomato soup. The liver is an amazing organ and has the ability to repair itself and due to Aaron’s home life that’s exactly what it did, his jaundice went, he was the healthiest he’d ever been and best of all he was starting to gain weight. He’d defied all the odds stacked against him!
In the summer of 1999 the doctors finally agreed that Aaron was fit and well enough to undergo his open heart surgery and it was performed at Birmingham. All went smoothly until like always seemed to happen to him, Aaron got a post op infection a particularly nasty fungal one and he became very poorly. His jaundice returned and his liver became very diseased once again.
The second transplant assessment took place January 2000 and Aaron was an urgent case due to the lack of venous access, most of his veins were "shot" meaning there was no access left for the IV line giving him his TPN, which was keeping him alive nutritionally. He was immediately listed for transplant and the rest was a waiting game, which we were very accustomed to.
On Sunday 29th May at 6 p.m. having literally just sat down to a Thai green curry and a glass of chilled Chardonnay, we got "the call", I don't think anything in this world can ever prepare you for it. We remained calm and got my sister to come and collect Jamie, we picked up our ready packed bag and went to collect Aaron who was in hospital, having just recovered from yet another life threatening line infection. The transport down was a light aircraft ambulance, there was lightning in the sky, it was freaky to say the least, and a crewmember told me not to worry if lightning hit the plane we’d be alright… AAAH! Fortunately when we arrived at the hospital the organs gifted were a match albeit the donor child was aged 10 years and Aaron was only 3 years meaning his liver needed to be reduced to fit, he was in theatre for about 12 hours, when we saw him the next morning we immediately noticed his colour changed back to a healthy pinkish tone his yellow jaundice had gone!
Very quickly he began to eat food properly, something we had never thought our son would ever do, he became IV free just 2 weeks post-transplant breaking the time record for this step, at that time.
A year post transplant Aaron developed a cancer related disorder, a b-cell lymphoma of his duodenum, triggered by EBV (Epstein Barr virus) and the immunosuppression medication he needed, called PTLD (Post transplant lymphoproliferative disorder) which was successfully treated with MabThera (Monoclonal antibody therapy)
Aaron is now 16yrs old, 12yrs post-transplant this year, he is leading a wonderful “normal” life, he can eat for Scotland. Though his medical history has left him with learning difficulties, he is doing really well at school. He's taken part in The British Transplant Games for 9 years in a row and won a few medals. He enjoys playing the drums, he plays football for a local team, mountain bikes locally and has been snow boarding in the Swiss Alps (on his own) to TACKERS (Transplant Adventure Camp for Kids) on several occasions.
He is such a typical teen lad and has such a strong outgoing personality, without which I’m sure he wouldn’t have made it through these past years, he is such a wee battler and even though he can drive us demented at times, he is forever an inspiration to us all. Aaron has his chance in life thanks to that most precious of all gifts the "Gift of Life" thanks to Aaron’s donor & his family, without their generous and selfless act upon the tragic untimely death of their son, Aaron would not be here with us today to enjoy this wondrous world of beauty and adventure…
Catriona (Aaron's proud mum)
This article is reproduced in full from Catriona's website Transplant Kids.
Imogen's Story
Imogen was born with a rare condition known as Myopathic Intestinal Pseudo Obstruction which ultimately resulted in her suffering from severe intestinal failure.
She was unable to process or absorb sufficient food to sustain life. Through a fine catheter that had been surgically inserted into a large vein close to her heart, a specially formulated “food” known as parenteral nutrition or PN was administered. This involved her being attached to an intravenous pump for a minimum of twelve hours each night. During her early years, she managed well on this regime. She was an active and lively young girl who enjoyed horse riding and walking her dogs but as she reached her early teens it became difficult to maintain her hydration and in addition to the parenteral nutrition, she required increasing amounts of saline to be administered intravenously. This meant that she was being connected to the pumps for longer periods of time.
By the age of thirteen she was experiencing considerable amounts of pain and was being connected to her pumps for between 18 and 23 hours a day so was unable to attend school. Home tuition was provided by the local education authority but she was isolated from her peers.
With time the repeated episodes of pain became more frequent and more severe. Emergency surgery was performed more than once and her doctors appeared helpless to improve matters. By the time she was sixteen, she was requiring around 6 litres of saline to be infused in addition to her parenteral nutrition each day and she was rarely having more than an hour or so free of her pumps. She was unable to walk very far due to the pain and was no longer riding. She was housebound and isolated and she appeared to be losing any confidence of a future. She worked hard at her school work and achieved good GCSE grades in all subjects despite being in so much pain at the time of her exams.
In July, 2009 Great Ormond Street Hospital discussed the possibilities of Imogen being put forward for a bowel transplant. We were taken to meet the consultant at Kings College Hospital where they had just started performing this type of transplant. At first we were very cautious since it is still a relatively new and uncommon procedure but it was decided that it was her only real choice.
She was put on the waiting list mid December 2009 and she received her transplanted bowel and pancreas on New Years Eve, just a fortnight later.
She remained in Kings College Hospital in London for around three weeks after the surgery and then spent a further month in a flat close to the hospital in order that she could be closely monitored with regular blood testing and occasional infusions. I was able to stay with her throughout and her Dad and sister visited whenever possible but it was hard being 250 miles away from home.
Once home, much of the following year was spent driving to and from London for Imogen to attend routine appointments or for unplanned admissions.
Imogen is now 18 years of age. She is able eat normally and no longer needs to be connected to pumps. She still requires close monitoring but generally this can be managed by the local hospital, though she will need to return to Kings College Hospital from time to time. It has been a long and hard journey for her since her transplant but she is now beginning to adjust to her new life and to plan for a future she thought she would never have.
Felicity, Imogen's mum.

Ronnie's Story
Ronnie was fine at birth but suffered a diaphragmatic hernia at the age of 14 months and lost all his small and half of the large bowel. After 4 years TPN dependent, Ronnie had his transplant in March 2011 at Kings College Hospital London.
Ronnie has done so well following his intestinal transplant that he took took part in this year's Transplant Games at Medway. Ronnie competed in the obstacle race, the ball throw, the 50m dash and the long jump. Phew!

